Dr. Anthony Chang’s Vision for Artificial Intelligence in Healthcare
At a time when the U.S. faces declining life expectancy and soaring healthcare costs, Dr. Anthony Chang delivered an urgent and energizing keynote at a recent health innovation conference. A pediatric cardiologist and Chief Intelligence and Innovation Officer at Children’s Hospital of Orange County, Dr. Chang is also the founder of AI Med and a thought leader in the convergence of artificial intelligence and medicine. His talk, both sobering and inspiring, offered a sweeping vision of how AI will transform healthcare over the next decade.
The Current Crisis and the Need for AI
Dr. Chang began by addressing the stark reality: for the first time since World War II, younger generations in the United States are expected to have shorter lifespans than their parents. Public health alone, he argued, cannot shoulder the burden of reversing this trend. “That’s a big lift for humans,” he said. “So what can we do in terms of using artificial intelligence to be what I call the equalizer?”
His framing of AI as an equalizer set the tone for the talk: AI isn’t about replacing doctors—it’s about empowering them. In a world where health outcomes are shaped by complex social, economic, and biological variables, AI can offer tools for pattern recognition, decision support, and scalability that are simply beyond human capacity alone.
From Generative to Agentic AI
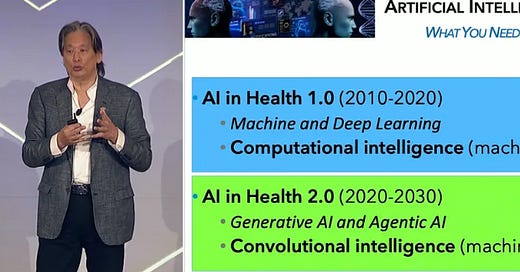
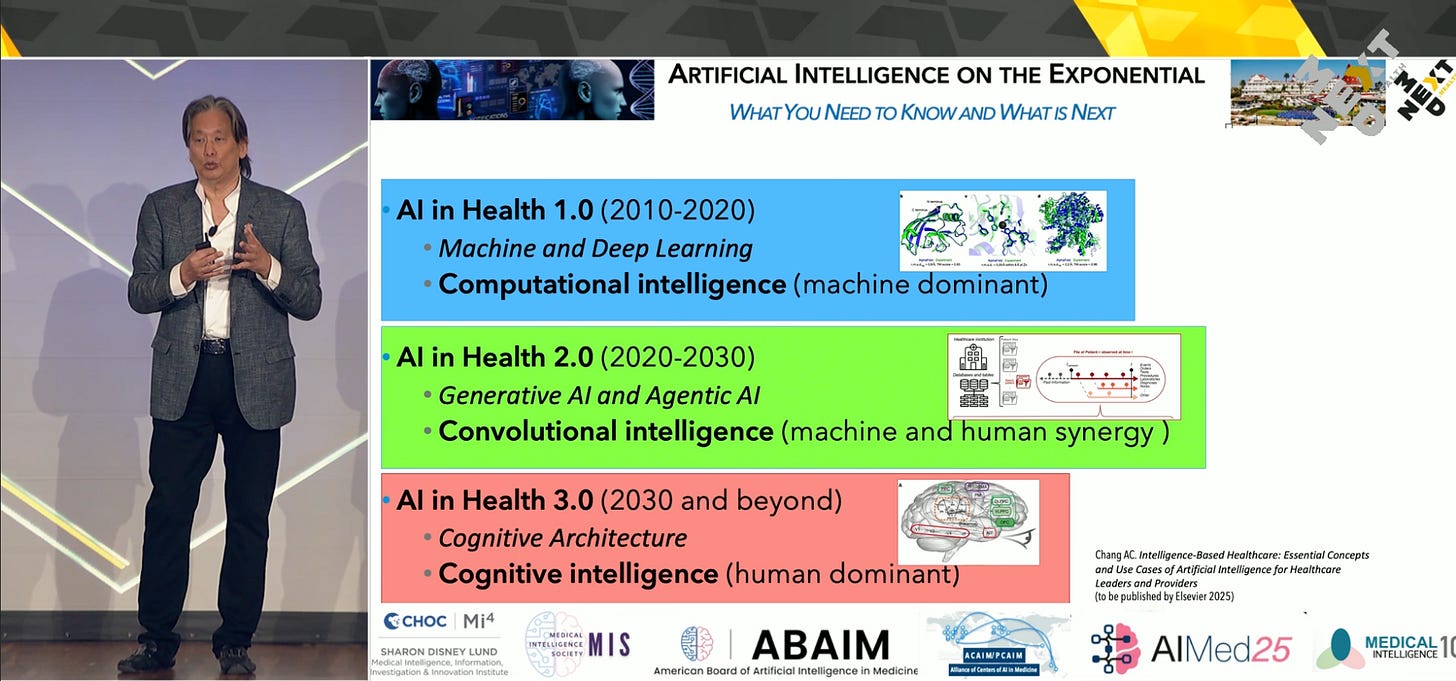
Dr. Chang traced the evolution of artificial intelligence in healthcare from what he calls “AI 1.0”—primarily machine learning and deep learning used in medical imaging—to today’s “AI 2.0,” where generative and agentic AI are taking center stage.
Generative AI, such as ChatGPT and DeepSeek, works like a coach—advising, summarizing, and responding based on vast internet-based knowledge. In contrast, agentic AI operates more like a quarterback on the field, with autonomous capabilities to take actions, adapt to changing environments, and direct tasks.
This metaphor resonated strongly: generative AI offers wisdom, but agentic AI brings execution. The combination of the two—when supervised properly—presents the most powerful opportunity to transform healthcare.
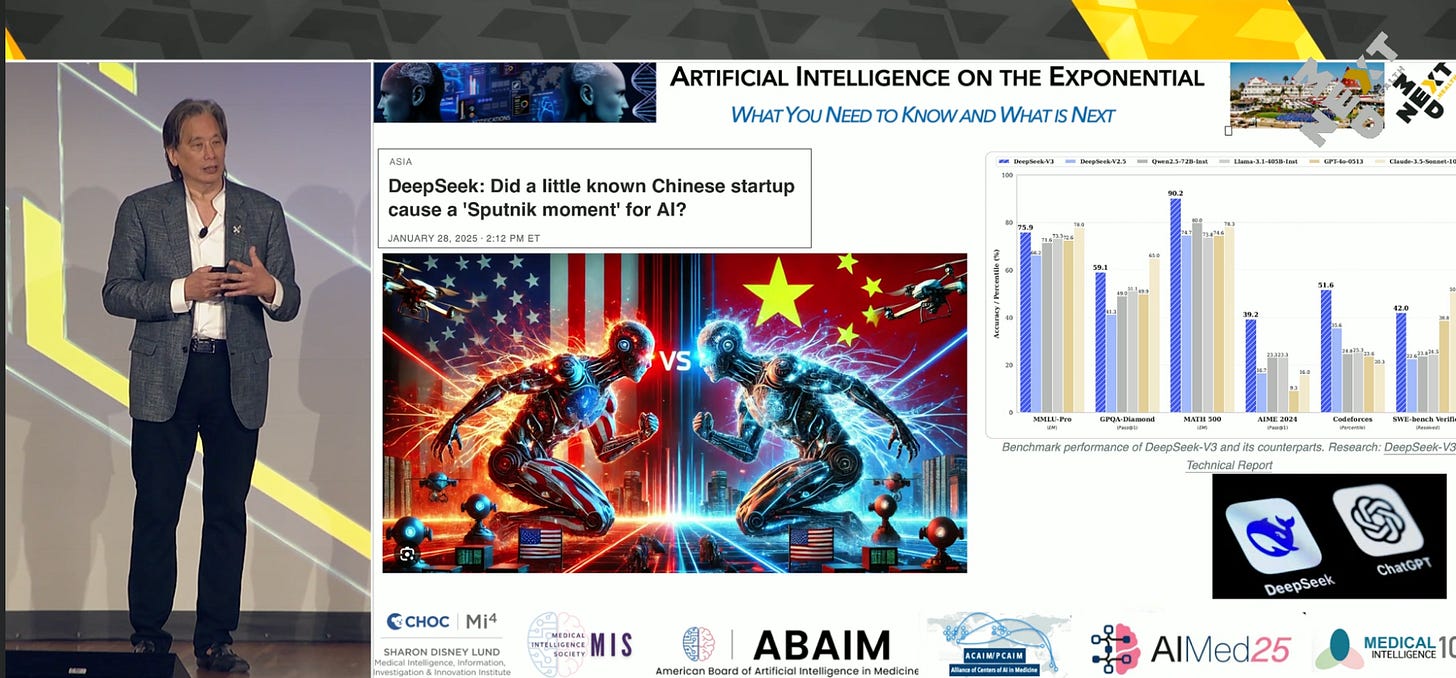
A recent breakthrough, DeepSeek, a Chinese startup’s large language model, was highlighted by Dr. Chang as a “Sputnik moment” not necessarily for AI in general, but for how accessible and democratized it has become. Its sophistication challenges the assumption that only trillion-dollar U.S. tech giants can dominate the space. As AI becomes more affordable and scalable, smaller hospitals and startups can meaningfully participate in this technological revolution.
Over 1,000 FDA-Approved AI Devices—But Uneven Distribution
Dr. Chang surprised many in the audience by revealing that there are already over 1,000 FDA-cleared or approved AI tools in healthcare today. The vast majority are concentrated in cardiology and radiology, highlighting a systemic imbalance in how AI is being applied.
He warned of multiple forms of bias and inequity—not just in the data used to train AI models, but also in how AI innovations are prioritized. Rare diseases, underfunded conditions, and low-revenue specialties are often left behind in the AI rush. "Bias doesn't just look like race or gender. It can be economic, geographic, or disease-specific," he noted.
From Medical School to Transformers: Understanding AI Architecture
For those newer to AI, Dr. Chang demystified how large language models (LLMs) like ChatGPT work. He likened the "pre-training" phase to a medical school education—broad, generalized, and expensive. The "fine-tuning" process, which adapts the model to specific tasks, is more akin to residency.
The real game-changer, he emphasized, has been the transformer architecture that underpins models like ChatGPT and DeepSeek. Combined with natural language processing (NLP), transformers allow LLMs to reason, contextualize, and produce responses that often feel eerily human.
Yet even the most advanced LLMs fall short in two critical areas: they lack access to full-text scientific publications and cannot read electronic health records (EHRs) due to privacy barriers. If clinicians and patients were willing to share more structured data and clinical wisdom, the potential benefits could be exponential.
A Glimpse into the Future: Cognitive AI and Digital Twins
Dr. Chang outlined a roadmap for the future of AI in medicine, moving from today's "computational intelligence" to what he calls "cognitive intelligence"—AI that can think and reason more like a human.
This future includes the use of digital twins—personalized, data-rich virtual models of individual patients. These could allow clinicians to simulate multiple treatment plans simultaneously and select the one with the best predicted outcome. Paired with reinforcement learning, this approach would replace today’s generalized clinical trials with highly personalized medicine.
"Imagine if your diagnosis or treatment could be tested on your digital twin first," he said. “We’re within a decade of making that happen.”
The Healthcare Nervous System
Perhaps the most profound idea in Dr. Chang’s talk was the call for a “healthcare nervous system.” This would be a real-time, globally connected system for sharing anonymized patient data. It would eliminate outdated, static textbooks and replace them with dynamic, evolving medical knowledge powered by real-world patient data.
“In the future,” he said, “medical students won’t learn from books. They’ll learn from living, breathing, constantly updated global data sets. That’s not science fiction—it’s technically possible right now.”
However, such a system will only materialize if patients, clinicians, and institutions agree to share their data responsibly and securely. Data governance, privacy, and consent will be central to making this vision a reality.
Regulating AI: Walking the Tightrope
Innovation in AI comes with regulatory and ethical challenges. Dr. Chang stressed the need for balance: overregulation can stifle innovation, while underregulation risks patient safety. He likened the AI development curve to a zigzag line on an exponential graph—progress is fast, but not smooth.
"Imagine driving a car with someone who brakes and accelerates unpredictably," he said. "That's how AI is evolving. Regulation needs to match that reality."
He also raised questions about future tariffs and FDA delays affecting U.S. innovation, particularly for startups that rely on timely approvals.
Strategic Advice for Innovators
For entrepreneurs in the room, Dr. Chang offered three core strategies:
Partner with Health Systems: Whether it’s a major hospital or a small clinic, having a strategic partnership is key to getting real-world feedback and clinical validation.
Focus on Data Governance and Validation: AI tools are only as good as the data and feedback loops they rely on. Innovators must prioritize clinical rigor.
Capitalize on Inefficiencies: The U.S. healthcare system, with its bloated administrative overhead, is ripe for disruption. AI can dramatically reduce waste if applied smartly.
Toward a “Smart AI” Era
While some fear artificial general intelligence (AGI), Dr. Chang emphasized that the real transformation will come not with a bang but with a whisper: when AI becomes so embedded in healthcare that we no longer talk about it.
“The lunar landing moment for healthcare AI,” he said, “will be when we stop talking about it at all. It will just be everywhere.”
He called this phase “smart AI”—an era when machine intelligence and human clinical wisdom converge to create systems that not only diagnose but understand context, nuance, and ethics. Clinicians will be more essential than ever—not just as decision-makers, but as collaborators and designers of these systems.
Final Thoughts and an Invitation
Dr. Chang ended on a personal note, inviting attendees to engage more deeply with the field. Through the American Board of AI in Medicine (abaim.org), he offers monthly crash courses for clinicians and innovators eager to learn how to apply AI to real-world problems. He also encouraged participation in the upcoming AI Med 25 conference in San Diego, a sister event to the NextMed Health summit.
Above all, Dr. Chang left attendees with a sense of responsibility. AI will not magically fix healthcare. It will take intentionality, interdisciplinary collaboration, and an ethical commitment to equity and access.
As he concluded: “Whatever your job is, if you’re now enlightened about artificial intelligence, you’re in a better position to keep that job—and transform it—than someone who ignores what’s coming.”